The Doctor Will See You Now

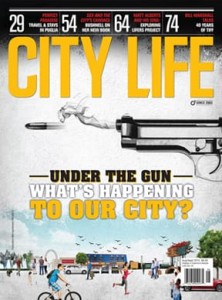
Physicians are expected to act in the best interests of their patients. But do they all?
How would you rate your family physician? Your surgeon? Your psychiatrist? Have you ever questioned his or her standards of practice, methods of treatment or diagnoses? When you leave your doctor’s office, are you confident that all your issues have been addressed to the best of your doctor’s ability?
If you are of a certain age, you may remember that there was a time when no one would ever think to question a doctor’s professionalism or expertise — not even a fellow professional. The doctor was sacrosanct. Along with priests and policemen, doctors were figures of authority whom the general public would entrust with their lives.
And so, it is with both surprise and alarm that we sometimes learn of incidents of fraud, overbilling, inappropriate sexual conduct and sexual impropriety on the part of society’s most trusted and vaunted figures, our doctors. As patients and advocates for both ourselves and our family members – husbands, children, elderly parents – what are the steps, questions and resources we need to be aware of in order to protect our loved ones?
The first question we need to have answered is, how rare are these charges? Or, conversely, how common are they? Are doctors ever found guilty of abusing their clients or the medical system itself? What recourse do patients have who feel that their doctor has acted inappropriately and below the anticipated standard of what they as patients expect from the doctor?
To answer these questions, it is important to understand the fundamental keystones of a doctor’s mission, and his or her purpose as a healer, not just from a physical aspect but from an emotional one as well. Historically, the time-honoured ritual for medical students, when they became physicians, was to take the Hippocratic Oath, possibly one of the most famous of ancient Greek medical documents. For centuries, new physicians swore to all the healing gods that they would uphold a number of ethical standards.
The Oath, which dates back to the 5th century B.C., has been rewritten over the centuries to suit the values of different cultures influenced by ancient Greek medicine.1
A fundamental part of the Oath states, “Into whatever homes I go, I will enter them for the benefit of the sick, avoiding any voluntary act of impropriety, of corruption, including the seduction of women or men…. In purity and according to divine law, I will carry out my life and my art.”2
The swearing of the Oath is not mandated in contemporary medical schools, but nonetheless it remains the ethical cornerstone of the medical profession. In the current version, new physicians swear by “whatever each of us holds most sacred.” All versions, regardless of amendments, promise the doctor will “act in the best interest of the patient and to protect patient privacy.”3
However, many of us, in our roles as patients or advocates, have read about, or even experienced, situations that are at the polar opposite of a physician’s sworn oath to act in the interests of a patient’s well-being. In fact, inappropriate behaviours by physicians have been known, and proved, to have taken place in our own backyards.
Dr. Rodion Andrew Kunynetz, a dermatologist practising in Barrie, was on March 21, 2017, found, by the Discipline Committee, to have committed an act of professional misconduct, in that he engaged in sexual abuse of a patient; engaged in conduct or an act of omission relevant to the practice of medicine that, having regard to all circumstances, would be reasonably regarded by members as disgraceful, dishonourable or unprofessional conduct. The investigative committee found no clinical justification for the sexual touching of the female patient. Two other patients alleged that Kunynetz moved or removed their clothing without adequate warning or explanation. And two more patients testified at a College of Surgeons and Physicians of Ontario (CPSO) hearing that Kunynetz had pressed his genitals against their legs. Kunynetz’s defense was that his lower abdomen was too fat for this action to be physically possible.
While the Committee did not find there was intentional touching against two of the patients, the investigative committee concluded that this supposed impossibility of contact with other complainants was not established. The Discipline Committee ordered the revocation of Kunynetz’s certificate of registration, as well as a reprimand and reimbursement to the College for funding provided to patients required under Section 85.7 of the Code, in the amount of $16,060, and payment of costs in the amount of $145,460.4
Certainly, not all misconduct by doctors has to do with sexual impropriety. Dr. Ranjit Kumar Chandra, a pediatrician practising in the field of allergy medicine, was found by the College, in March of 2016, of submitting and having unusual billing patterns and referral sources regarding his billings. The College received a complaint from Patient A, who had only seen Dr. Chandra on one occasion, that he had asked her to participate in a fraudulent billing scheme using her health card and those of her family for services he had not provided. Patient A also heard Dr. Chandra approach other patients to the same effect. Three other patients testified at the hearing and the Committee considered detailed documentary evidence including OHIP records, Dr. Chandra’s banking records, his records from Rogers Communications and Bell Canada, as well as email correspondence seized by the College.
The evidence demonstrated that Dr. Chandra recruited approximately 300 people to this scheme, and $2,056,342 in OHIP fees were paid to Dr. Chandra over four years. Dr. Chandra was found by the Committee to have engaged in a scheme to defraud OHIP, including soliciting patients to participate in the scheme, and providing patients with payments in exchange for their participation in the scheme.
The Committee ordered the revocation of Dr. Chandra’s certificate of registration, a $35,000 fine payable to the Minister of Finance, and a reprimand. Dr. Chandra was also ordered to pay costs to the College in the amount of $16,500. 5
Disquieting as the details of such charges are, it is important to understand the scope of the issue, the processes in place for patients to file complaints, the factors that the CPSO’s Inquiries, Complaints and Reports Committee (ICRC) considers when examining each complaint, the accountabilities and consequences imposed on offending physicians, and the after-support provided to the victims of these sexual assaults.
To understand the scope of the sexual abuse and sexual impropriety complaints brought to the CPSO, one must look first at the number of overall complaints filed against doctors over the last few years (including issues such as overbilling and incompetence to practice), then at the breakdown of subsequent cases proven after an ICRC investigation.
In 2017 (the last year for which the CPSO has stats), there were 2,682 new public complaints, of which 691 went to the ICRC. Of those, 45 cases of various transgressions such as sexual abuse, sexual impropriety, incompetence and failure to maintain standards were proven. Of the 45 cases, 11 per cent (6 cases) were proven transgressions of sexual abuse, and 2 per cent (1 case) was a proven sexual impropriety. The sexual impropriety charge landed the physician a revocation. The sexual abuse charges resulted in three revocations and two suspensions.6 In 2016, of 46 proven cases, 28 per cent (13 cases) were for sexual abuse. There were 84 referral cases before the committee at the end of 2016; 35 per cent (29 cases) were for sexual abuse; 2 per cent (2 cases) were for sexual impropriety.7
Of the 31 proved cases in 2015, 19 per cent (6 cases) were for sexual abuse, and 3 per cent (1 case) was for sexual impropriety.8 The facts of complaints of sexual abuse and sexual impropriety are highly unsettling. The public should be aware of what is being done to identify and prosecute offending doctors. First, the CPSO has a Complaints Process in place for patients to register their complaints. The CPSO website also lists a doctor’s status (in good standing or restricted licence) in its Find a Doctor database. There is also a current ongoing list of Unregistered Practitioners who fraudulently claim to be doctors. (Visit www.cpso.on.ca/Public/Services to access all the resources described in this paragraph.)
“Physicians today are more collaborative with their patients. But I believe that the public have to be their own advocates, and that patients have to be informed and involved in their own care” − Cheryl Behan
The College’s ICRC considers a number of different factors when reviewing and investigating complaints. These include: the facts of the case; the number and seriousness of care/conduct concerns at issue; whether the physician is practising within his or her area of expertise; the physician’s response to the investigation; physician insight; the physician’s self-identification of areas for improvement and changes to practice; the physician’s apparent capacity for remediation; the physician’s investigative and disciplinary history; expert opinions obtained in the course of the investigation; and other doctor and witness information.
“The College (of Physicians and Surgeons of Ontario) takes complaints from the public very seriously and follows up on them with due process. They do a good job on that front, with respectable checks and balances in place,” says Cheryl Behan, retired assistant head nurse of the Neurosurgery Unit at St. Michael’s Hospital, Toronto, as well as a member of Orillia’s Soldiers Memorial Hospital CEC (Community Engagement Committee). “Quite often, complaints are dealt with at the first level, between patient and doctor; if a complaint escalates to the College (CPSO) level, it is very, very serious.”
And while 33 per cent of open investigations involve a physician with more than one active investigation, it is comforting to know that the median number of days to complete an investigation decreased 18 per cent between 2016 and 2017.9 The ability to identify, isolate and discipline in a timely manner a physician who is dangerous to public safety is crucial to ensuring the ongoing confidence of patients.
“If the complaint is minor, I think the patient should speak up and address it with the physician or his administration,” Behan says. “It can be done in a diplomatic way. If, however, it is a major complaint, I believe it is the patient’s responsibility to let the physician know the seriousness of the complaint and that they want it resolved. If the physician does not agree with the patient’s complaint, that is when the patient can discuss it with the manager or, conversely, the patient can call the CPSO.”
Certainly, media spotlight on the impropriety of some doctors’ conduct is unforgiving. It is also important that doctors who are unfairly accused have their own processes of protection. “The investigative process is a fair process intended to identify the truth and address concerns by obtaining relevant information, including medical records (from the doctor or other health care providers or facilities) and other documents. The investigator may interview witnesses, including family members, pharmacists, nurses, other doctors involved in the care, and hospital administrators,” says Shae Greenfield, senior communications advisor at CPSO.
The trauma of being sexually abused by a trusted figure is intense and far-reaching. Feelings of fear, confusion, anxiety, mistrust and, in some cases, guilt can haunt a patient for years. Through its Patient Relations Committee, the CPSO offers assistance in the form of funding for therapy and counselling to patients who are found by the College to have been sexually abused by an Ontario physician, or whom the physician admits to having abused, or whose physicians are convicted under the Criminal Code of Canada for sexual abuse.
Certainly, doctors are not the only ones in the patient-care field who engage in sexual impropriety. One recent case is that of massage therapist Jasil Rahman Puniyanikodan, who was convicted of sexual assault earlier this year. Which raises the question: How can the public protect themselves against sexual impropriety from health care providers (including doctors, nurses, dentists and medical support service providers)? And can we, as patients, continue to place our trust in the medical field?
For entry into the MD Program, the University of Toronto requires applicants to submit to a Vulnerable Sector Screening and Criminal Record Check as a condition of their registration, with an annual “attestation” in subsequent years of the program. All new domestic postgraduate medical residents and fellows must submit the results of a Vulnerable Sector Screening as a condition of their registration in the program.10
Applicants to the College of Nurses of Ontario (CNO) must declare whether they have any condition, disease or disorder that could impact their ability to safely practise nursing. “They must also declare any ongoing proceedings, criminal charges and/or findings by lawful authorities,” says Farah Ismail, director, Professional Conduct, CNO. “The CNO reviews all information received during the application process to ensure that applicants meet the conduct and health requirements.”
While there is no official psychological testing for physician or nursing candidates, the CNO has a new Code of Conduct for nurses that specifically outlines the expected behaviour and accountability nurses must adhere to, including maintaining professional boundaries. “At the core of nursing is the therapeutic nurse-client relationship,” says Ismail. “Recognizing that boundary violations can lead to sexual abuse, both the Code of Conduct and the Therapeutic Nurse-Client Relationship Practice Standard clearly identify the need to maintain the appropriate boundaries. In addition to sexual abuse, the College’s abuse prevention program addresses physical, verbal and emotional abuse.”
Disturbing though they are, news stories of abuse and impropriety and intense media scrutiny on misconduct should not be seen as a massive breach of public trust.
“When you think of all the hours, and all of the surgeries, and all of the patients that doctors see, I don’t believe these types of incidents represent a big number,” Behan says. “What I think is that we hear about the serious cases nowadays. And that is good. It keeps the public informed and aware that there are systems in place to report inappropriate behaviour or activity. Physicians today are more collaborative with their patients. But I believe that the public have to be their own advocates, and that patients have to be informed and involved in their own care.”
Footnotes 1, 2: National Library of Medicine (2002), translated by Michael North
Footnote 3: UCLA David Geffen School of Medicine
Footnotes 4, 5: MD Dialogue Magazine, Volume 14, Issue 4, 2018
Footnotes 6, 7, 8, 9: College of Physicians and Surgeons of Ontario, (CPSO) Annual Reports
Footnote 10: Professional Association of Residents of Ontario (PARO)















No Comment