How a Child’s Breathing Problem Can Be Misdiagnosed as ADHD
Dr. Ami Barakat shares his insight into how misdiagnosis can occur and what parents should be aware of should their child be labelled with ADHD.
Written By Dr. Ami Barakat
They are two conditions that might seem to have nothing in common: mouth breathing and Attention Deficit Hyperactivity Disorder (ADHD).
Yet children who breathe through their mouths because of a dental issue may be easily misdiagnosed with ADHD, resulting in a lifetime of being given powerful drugs unnecessarily.
“Mouth breathing is often caused by an obstruction in the nasal airway,” says Dr. Ami Barakat, a dentist and author of Perfecting Smiles, Changing Lives. “More than half of the people diagnosed with ADHD are mouth breathers. That is too significant a statistic to be a coincidence.”
In the case of ADHD, a dental exam can also prevent a misdiagnosis which can have lifelong impacts
In the United States, anxiety disorders such as ADHD are the most common mental illness, affecting 40 million adults, according to the Anxiety and Depression Association of America. Meanwhile, ADHD is the most prevalent psychiatric disorder in children in Canada, according to the Centre for ADHD Awareness, Canada. Conservative estimates suggest that 5 per cent of Canadian children are affected, and the number of diagnoses has risen dramatically over the decades along with the number of children being medicated.
Mouth breathing can result in a lack of oxygen saturation in the brain, Dr. Barakat says. Mouth breathers are more likely to have cerebral hypoxia or a reduced supply of oxygen to the brain. And mouth-breathing children get a low quality of sleep, which affects their mood, ability to focus and behaviour at school. Dr. Barakat says this can easily be confused for ADHD.
Other impacts on children who are mouth breathers include:
1. Snoring
2. Teeth grinding
3. Nightmares
4. Bedwetting
5. School issues (due to lack of sleep and possible low oxygen to the brain, they may appear lazy, have trouble focusing, etc.)
“Every diagnosed case of ADHD can’t be eradicated with solving mouth-breathing issues,” Dr. Barakat says. “But the parents of children who are mouth breathers and have been diagnosed with ADHD should get a second opinion from a dentist or orthodontist before accepting the ADHD label. Once a child has that label, it usually means they will take powerful drugs such as Ritalin or Adderall for the rest of their lives.”
ADHD is such a common issue with dentists that the American Dental Association (ADA) has issued some guidelines about how to handle those patients with ADHD, including asking dentists to look for signs of physical abuse.
“Abuse is more common in children with developmental disabilities and often manifests in oral trauma,” according to the ADA. The association says if dentists suspect physical abuse, they need to report it to the proper authorities.
It also warns dentists that children with ADHD frequently will go without medication during times they are not in school, so they should be sure to ask if the child has been on medication.
It suggests dentists delay treatment for any child who has not been on the proper medication.
Children with ADHD generally have poor dental health and frequently have increased behaviour management issues when visiting the dental office.
The ADA has given dentists guidelines on how to handle a child with ADHD in the office:
1. Schedule appointments in the morning or at a time of day when the child is least fatigued, most attentive and best able to remain seated in the dental chair.
2. Give short, clear instructions directly to the child. Give only one instruction at a time.
3. Use the Tell-Show-Do approach when introducing new procedures. Tell the child what is expected of him/her during the visit.
4. Consider small rewards for appropriate behaviour (stickers, etc.). Positive reinforcement may be helpful in obtaining compliance.
5. Discuss appropriate behavioural interventions with the parent.
6. Determine if breaks are necessary during treatment.
7. Consider the use of nitrous oxide during treatment to manage behaviour.
Mouth breathing isn’t the only thing that can lead to a misdiagnosis of ADHD. Many of the lesser-known symptoms of ADHD — such as memory issues, difficulty sleeping and irritability — also show up with conditions such as mood disorders, autism, anxiety and other brain-based conditions.
Research also indicates that minorities are less likely to have a parent-reported diagnosis. This could possibly be related to a genetic advantage or a decision not to seek medical care for the symptoms (which could be related to cost factors, perceived stigma or not viewing ADHD as a true disorder).
In the last six years, the rate of diagnosis of ADHD has jumped 15 per cent according to data from the Centers for Disease Control and Prevention. That may influence more parents to accept that diagnosis before looking into other possible issues.
“New research has shown that dental issues can impact everything from back problems to headaches. But in the case of ADHD, a dental exam can also prevent a misdiagnosis which can have lifelong impacts,” says Dr. Barakat. “The old days of dentists only concerning themselves with filling cavities and lining up teeth are long gone.”
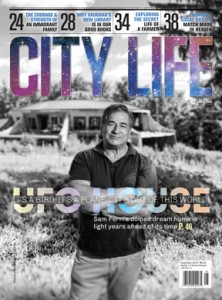
About Dr. Ami Barakat
Dr. Ami Barakat, author of Perfecting Smiles, Changing Lives, is a general dentist who has trained extensively in orthodontics. He has received several prestigious awards in recognition of his talent, achievements and passion for dentistry. He graduated from the University of Toronto Faculty of Dentistry with honours and served a one-year residency at the Royal Victoria Hospital in Montreal.
www.villanovadental.com


















No Comment