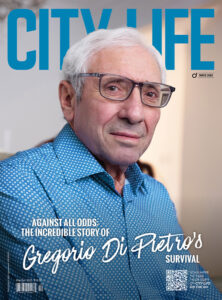
Unbreakable — Paul De Lio
Paul De Lio almost didn’t make it — he was inches from death. This is a story of unimaginable strength, inspiring family bonds and one young man’s will to live against all odds.
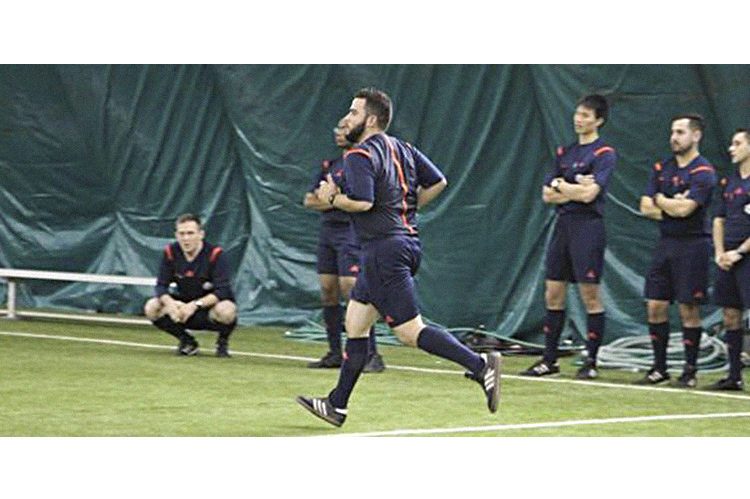
When Paul De Lio was admitted to The Scarborough Hospital-Grace Division’s intensive care unit on April 30, he was listed as the sickest person in all of Canada. His heart stopped for three entire minutes — his body was in shutdown mode. It was nearly a week — what seemed an eternity to the De Lio family — before doctors discovered, almost too late, which deadly bacteria had invaded Paul’s body. Paul was diagnosed with invasive group A strep. He spent three months in the hospital recovering from his near-death experience and the collateral amputation of both of his legs just below the knee. Paul was a healthy, athletic 30-year-old just prior to his illness.
Nerves are high before we enter the De Lio home. Unsure of what to expect, we prepare ourselves for an emotional interview, tissues in hand. To our surprise, the apprehension dissipates in an instant. Paul’s confidence and positive spirit fill the room with a sense of calmness and comfort. “Would you like an espresso, water?” asks Paul, as he manoeuvres around his basement apartment in his prosthetics. It’s hard to believe he’s been out of rehab only a month; the young amputee is adjusting to his new life with optimism.
Paul tells us what he was most passionate about: his role as an educator, coaching youth soccer and volunteering his time to teach catechism classes at local church for the past five years. He also gushes about his love for his four nieces and his nephew. Circumstances have changed, but he maintains that his dedication to the aforementioned hasn’t. He’s living proof that a positive mindset, an unbreakable support system and determination can pull you through anything.
It was Wednesday, April 26, and the young teacher was just beginning a new contract position at an elementary school when he asked to leave early because he was feeling ill. One of the last things Paul recalls is visiting a walk-in clinic for what presented as a “typical flu” and being sent home. “The doctor told me, ‘Take some fluids. Get some bed rest. Go home.’ What else are they going to tell you to do? That was that,” says Paul, who admits to being a good advocate when it comes to his health. But in just 48 hours, Paul’s innocent flu-like symptoms went from mild to lethal, and he collapsed in his home on Sunday morning. “I woke up in the hospital three weeks later.”
Frank De Lio, Paul’s older brother, fills in the gaps. As he begins to share Paul’s story, he takes a deep breath. Although his brother is alive, it’s without a doubt that Frank’s heart aches recalling the day that changed his family’s life forever.
“The doctor came over to talk to me and just said, ‘Your brother is very, very sick, and your family needs to prepare themselves. He could die today’”
“When we got to the hospital everyone was crying,” says Frank, with a crack in his voice. “The doctor came over to talk to me and just said, ‘Your brother is very, very sick, and your family needs to prepare themselves. He could die today.’” Paul’s organs were in distress simultaneously, and he had gone into cardiac arrest about 30 minutes after he arrived at the hospital. Struggling to stabilize Paul, the doctors put him into an induced coma — but the clock was still ticking on a diagnosis. “I remember going outside and just basically collapsing to my knees just crying; I couldn’t believe what was happening to my little brother.”
Paul’s lungs and heart were failing and his kidneys had already shut down — he was on life support. Dr. Niall Ferguson, head of critical care at the University Health Network, which includes Toronto General, was called in to see if Paul was a candidate for a procedure known as extracorporeal membrane oxygenation (ECMO), a lung bypass. ECMO uses a modified cardiopulmonary bypass circuit for temporary life support of patients with potentially reversible cardiac or respiratory failure, essentially buying doctors more time. Dr. Ferguson tells us that Toronto General is the only hospital in the region that performs this life-saving service.
“The doctors said Paul was a good candidate, but my parents needed to decide whether or not he would go through with it — there were a lot of potential risks,” says Frank. Grasping for any hope they could, Paul’s parents, Peter and Delia De Lio, gave the procedure the green light. The surgery was successful. “There was virtually no good news for the next few days because the doctors kept doing blood work to try to identify which bacteria it was,” says Frank. “They kept looking at his white blood cell count, and the infection was still there.” But the De Lios didn’t lose hope. Delia was by her son’s side day and night.
Doctors finally identified the bacteria as invasive group A strep, Paul was suffering from toxic shock; his blood was poisoned by the bacteria. According to the Public Health Agency of Canada, the vast majority of Strep A infections present as non-life-threatening conditions, such as strep throat. In extremely rare cases like Paul’s, the bacteria can infiltrate other parts of the body that it wouldn’t normally, such as the bloodstream — these “invasive” strep A infections can be life-threatening. Variations of invasive strep A include septicemia (blood poisoning), meningitis and necrotizing fasciitis, sometimes called flesh-eating disease.
“The doctors told us that 99.9 per cent of the time, the bacteria is completely harmless to humans,” says Frank. “We carry it on our skin, in our mouths. In this tiny percentage of people, it ends up being invasive and getting into where it’s not supposed to, and just attacking.”
Dr. Ferguson says invasive group A strep is quite acute; it comes on quite suddenly and is not easily predicted. “There is a significant mortality associated with it, because despite antibiotics (which are the cornerstone to treating bacterial infections), often the body’s own immune system has a huge response to the infection and it can be difficult to get under control,” says Dr. Ferguson. “We often need to support the lungs with a mechanical ventilator, the heart with adrenaline-type medications, and often the kidneys need help with dialysis — all those things were true in Paul’s case, plus he needed ECMO support.”
“I want to get back to coaching soccer and teaching, but I don’t want to be limited, which is why I haven’t been back yet”
It was about two weeks before Paul was taken out of the coma, and Frank says he was terrified of what his brother would see when he regained consciousness. “Because they had him on some strong blood pressure medication, the blood vessels in his legs, arms and in his extremities closed, and it pushed the blood to his core. He needed the blood at his heart and his lungs and his brain.” The De Lios were warned of the risk that Paul’s blood vessels could die, and that he could suffer from necrosis in his feet. It happened.
“I couldn’t talk much when I woke up, but I remember looking down at my feet and asking my brother what happened,” says Paul, miming the way he had anxiously gestured to his feet. “They were black.” Although his organ functions were slowly improving, his toes and feet were damaged beyond repair. “I remember as he was getting worse, we were begging, I was begging the doctor, ‘Please, there’s something you guys have to do. He’s an athlete. He’s a soccer player. He’s a teacher.’ Losing his feet is like the worst punishment he could get,” says Frank.
Paul’s attending physician suspected his immune system was expending large amounts of energy trying to repair his damaged feet, to no avail. “He expected his kidneys to recover after amputation as his body would focus on healing the other damaged areas, and it did,” says Frank.
After the amputation Paul’s recovery sped up.
Both of Paul’s legs were amputated just below the knee, and after two weeks of recovery post-surgery (“it was supposed to be six, but I’m an all-star,” says Paul), he was transferred to St. John’s Rehab at Sunnybrook Hospital, where he would spend two months as an in-patient and slowly transition back to his home with his prosthetics.
While at St. John’s Rehab, Paul was under the care of Dr. Amanda Mayo, a physiatrist with a subspecialty in amputee rehabilitation. Dr. Mayo is excited to share the progress Paul has made in the last few months and sheds some light on the challenges that Paul will face short-term and long-term.
“I think initially Paul was in shock, and I think it was very hard for him to be dependent on other people,” says Dr. Mayo. “He was very adamant that he wanted to be independent and he didn’t want to be disabled.”
This was understood from our meeting with Paul. The 31-year-old who lives in the basement apartment of his parents’ Scarborough home isn’t the type to rely on others. “Everyone tells me to reach out if I need anything, but I’m never the type to ask for help,” says Paul. “I was so independent before, I haven’t asked my parents for money since I was 17 — do you know what I mean?” Very few modifications have been made to the home to accommodate his new challenges and he’s happy this way — for now.
Dr. Mayo shares that amputees are always at risk of getting skin breakdown or knee pain, back pain and hip pain. They have an overall increased risk of wear and tear on their bodies because the prosthetics are quite heavy and require time to feel comfortable with. “That will be probably longer down the road; that’s why we’re encouraging Paul,” says Dr. Mayo. “Impressively, he’s quite motivated to keep as strong and active as he can.” Paul is currently attending physical therapy twice a week and visits Scarborough General once a week for finger therapy — due to the lack of blood flow, mobility in his fingers was severely hindered.
Paul says he follows a lot of motivational pages and amputees on Instagram now. “There are amputees who are ripped,” says Paul. “It’s like, ‘Holy crap, how are you doing that?’ but it’s just that there’s nothing stopping them. The stronger you are, the more things you can do, and the more you can handle this.”
“I think it’s a difficult journey and I wish all patients were as successful as Paul,” says Dr. Mayo. “Patients like Paul are inspiring to the other amputees that he comes across.”
Another reality that is often overlooked is the financial hardships that amputees will face. For Paul, this means outfitting his home with support bars, purchasing a modified vehicle, high insurance premiums, physical therapies and a new pair of prosthetics every three years. “Paul’s legs are, I would call them, average type legs that he purchased; they’re not for running or walking on the beach,” says Frank. “They cost just over $20,000, and OHIP only covers 75 per cent of a basic, basic pair — for Paul this is only about 25 per cent.” In addition, Paul is an occasional teacher with the school board and didn’t have basic health care benefits at the time of his illness.
The De Lios have started a fundraising campaign for Paul on www.FundRazr.com to assist with these amassing expenses. To date, the donations have surpassed $150,000, and the page is filled with messages of encouragement from friends, family, colleagues and students. Paul touched so many lives as an educator, and his impact was widespread.
How is Paul today? Doctors say the full extent of damage caused by the bacteria will reveal itself over the course of six to 12 months, however, Paul is expected to make an 80 to 90 per cent recovery (never getting 100 per cent of his lung capacity back). “To my surprise, to my family’s surprise, my brother has been such an inspiration to us, because his attitude has just been absolutely amazing,” Frank says. “You know, people ask me how my brother is doing. My response is, ‘My brother is a stud. My brother is a champ,’ because I don’t know if I would have had the capability to handle it the way he handled this. You know, I’m so proud of him. I’m just so, so, so proud of him.”
Paul shares that he is anxiously awaiting the day he can get back to living his life and hopes to put the past behind him — he’s getting a little bored of watching TV all day. “I want to get back to coaching soccer and teaching, but I don’t want to be limited, which is why I haven’t been back yet,” says Paul. “I could go back today, I can be there right now, but I would walk at a snail’s pace.” He contemplates the small challenges he’ll face if he rushes the process, like stairs or changing his shoes in the winter. Paul wants to be prepared. “I don’t want any favours,” he adds. His fierce independence is inspiring. He even manages to crack a joke or two about his legs to keep the mood light.
Paul’s words of wisdom: “There are always other things you can do in life; you’ll always find new things that you can do. Try to find your motivation to allow you to do whatever it is that you want to do in life.”
Without a doubt, with his family by his side, Paul will continue to persevere and be a prime example of courage and strength for all those he meets.
photos courtesy of Paul de lio























No Comment