Debunking Common Misconceptions About Crohn’s & Colitis
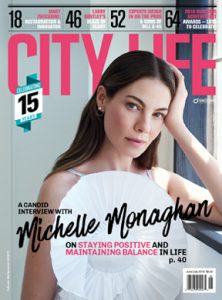
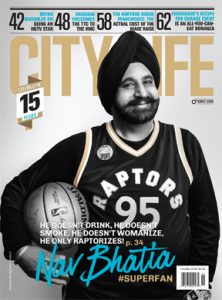
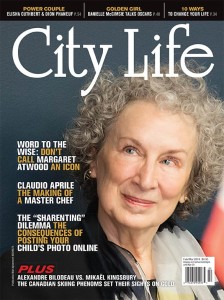
Canada has among the highest rates of Crohn’s and colitis in the world. We spoke with Dr. Kate Lee, vice president of Research & Patient Programs at Crohn’s and Colitis Canada, to understand why.
The last decade or so has marked a sea change in how we collectively think about and discuss mental health issues, particularly about the cascading effects that physical illness or disability can have on our mental well-being. Crohn’s disease and ulcerative colitis, conditions that affect the bowel, sit at the intersection of these historically disparate areas of medicine, particularly regarding the significant lifestyle changes, embarrassment and depression that tend to result from their physical symptoms. As Dr. Kate Lee, vice-president of Research & Patient Programs at Crohn’s and Colitis Canada, explains, “People living with Crohn’s or colitis are twice as likely to develop mental health issues, especially anxiety, compared to the general population.”
“The stories you hear about how Crohn’s or colitis has affected people’s lives are heartbreaking. These diseases impact all aspects of an individual’s physical and emotional well-being and can be quite isolating. When someone is in a flare, they stay home, they can’t do anything. They’re even afraid to go grocery shopping because of the unpredictable bowel movements. They even talk about how they’ve changed their career aspirations because of knowing that they’ve been diagnosed with this disease. Their social life and travel plans are definitely impeded — so many aspects of their lives are affected by this disease.”
Dr. Lee brings up the unfortunate prevalence among Canadians in of Crohn’s and colitis, diseases that are often hidden by those who live with them. “We predict about one percent of Canadians will have an inflammatory bowel disease by 2030. That’s not a small amount. It’s a disease that is out there, and I wouldn’t be surprised that if you start talking about it, you’re going to find out that you know people who have the disease.”
To understand more about the difference between IBS and IBD, as well as Crohn’s and colitis, we asked Dr. Lee to debunk common misconceptions about the conditions and hopefully shine more light on a condition that people all too often deal with in isolation.
Q: What’s the difference between irritable bowel syndrome (IBS) and inflammatory bowel disease (IBD)?
A: Irritable bowel syndrome is not a disease and it doesn’t involve your immune system. Inflammatory bowel disease has the word “inflammatory” and “bowel” in there because it involves your immune system. Irritable bowel syndrome is an intolerance to certain food groups. So, for example, I’m lactose intolerant because my digestive system doesn’t have enough of the enzymes needed to digest lactose. That’s why I developed an intolerance and why I get uncomfortable when I eat dairy products. There’s a very big difference between the two. With IBD, your own immune system starts attacking your own gut, causing all sorts of havoc in your digestive system, including ulcerations, bleeding, scarring, blockages and fistulas, where the gut has worn away completely and fuses with other organs or body surfaces.
Q: What is the difference between Crohn’s and colitis?
A: Our organization is called Crohn’s and Colitis Canada to really recognize that the two main forms of IBD are Crohn’s disease and ulcerative colitis. Crohn’s and colitis stands for Crohn’s disease and ulcerative colitis. They’re the two main forms of a group of diseases called inflammatory bowel diseases. The reason it’s called “bowel” is because it affects your gut — for Crohn’s disease, anywhere from the mouth to bum, whereas ulcerative colitis is localized in the large bowel. IBD is an autoimmune disease, so what happens is your immune system goes awry, and your own immune system starts attacking your gut. Unfortunately, there are no cures and it can happen at anytime in your life. There are children diagnosed with IBD and there are seniors who are diagnosed with IBD. Having said that, the time when most people get diagnosed with IBD, unfortunately, is during the “the prime of life,” between the ages of 16 and 30.
Q: What are some of the symptoms that people have with Crohn’s or colitis?
A: When it first starts, symptoms can be similar to your gastrointestinal system not feeling comfortable, and maybe having to use the washroom more often. Common symptoms include frequent and urgent bowel movements and bloody stools. When things escalate, if people don’t go see a doctor and get diagnosed properly, it could lead to severe malnutrition and sometimes death. Chronic fatigue is something that a lot of patients experience because of all the bloody stools and having to use the washroom so often, and they have chronic pain, again because their gut is all inflamed.
IBD is a progressive disease, which means that the longer you have it, the worse it gets. So, the key to treating it, and to ensure that you maintain a good quality of life, is to diagnose it early, and treat it early.
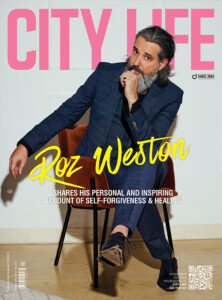
Dr. Kate Lee
Q: Is it a genetic disease, brought on by something that you eat or your lifestyle?
A: It’s a combination. We say that there have to be three factors, and they kind of clash together. And when they clash in a certain way, the individual develops the disease. There’s the genetic component, there’s the environmental component and then there’s our gut microbiome.
Q: What have scientists discovered about those three factors?
A: Scientists have identified more than 200 genes that are involved in IBD and some of the treatments we have target these genes. Scientist studying the microbiome have determined that the gut flora in people with IBD are different compared to healthy individuals. We also know that industrialization (pollution) is involved. Diet also probably plays a role. Emulsifiers found in many of our store-bought foods could play a part. But the challenge is that we still don’t know what is cause and effect because all studies have been conducted after the disease has developed or in animal models. And, although animal models are a great way to try to pull apart questions like cause and effect, discoveries do not necessarily translate to humans. The only human study in the world that is trying to determine the cause or causes leading to IBD is our GEM project which has been following healthy relatives where, because of their genetic link, a proportion of them will develop the disease. We’ve been supporting this study since 2007 and we still have a ways to go. In other words, our researchers have increased our understanding of IBD significantly, but we still have much more to do.
Q: Does hygiene play a role?
A: Yes, there’s also the hygiene hypothesis, where children living in developed nations tend to be less exposed to bugs such as bacteria and viruses while growing up. Exposure to bugs during a child’s development is an important part of teaching our immune system what are good and bad bugs. Since antibiotics kill all bugs, scientists also speculate that increased antibiotic use could be a factor in developing IBD.
Q: What is important to note about IBD?
A: IBD is a progressive disease, which means that the longer you have it, the worse it gets. So, the key to treating it, and to ensure that you maintain a good quality of life, is to diagnose it early, and to treat it early. The longer you wait, the worse it’s going to be for you. So, if someone has experienced ongoing symptoms suggestive of IBD, I would highly encourage them to go see their doctor.
To learn more about inflammatory bowel disease, visit: crohnsandcolitis.ca/not-alone
crohnsandcolitis.ca
@getgutsycanada