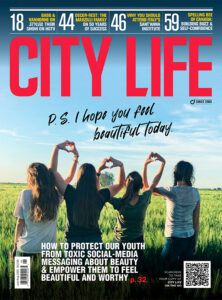
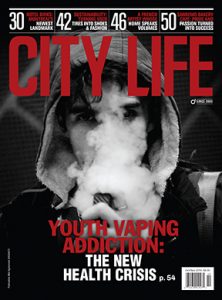
Youth And Mental Health: The Shadow Pandemic
The pandemic has had a detrimental effect on the mental health of our youth. They feel isolated and alone, without peer support or the usual engagement in fun activities. But there is help for this cohort that is free, anonymous and non-judgmental.
In the late 1960s, a popular public service announcement that ran on American television channels posited the question: “Do you know where your children are?” It quickly became a popular meme before that term was even coined, and it was often derided by the exact demographic to which it was targeted.
As we slouch toward the one-year anniversary of the COVID-19 pandemic, this 1960s question resonates once again. However, we are now parsing that query through the complex lens of a different kaleidoscope, one that focuses on the mental and emotional health of our youth, rather than their physical well-being and welfare. Fact: There has been an alarming rise in the number of kids who are going to the emergency department for eating disorders, mental health issues and self-harm behaviours.
Fact: It is an increase that ranges from between 50 per cent and 6o per cent. A Nov. 23, 2020, Ontario Student Drug Use and Health Survey (OSDUHS) Mental Health and Well-Being Report released by the Centre for Addiction and Mental Health (CAMH) reports that “Ontario students were experiencing the highest levels of suicidal ideation and serious psychological distress ever recorded.” The study identifies the data as being collected between November 2018 and June 2019 from among 14,142 students in Grade 7 through to Grade 12. The study goes on to say that suicidal ideation is currently the highest on record for this survey since CAMH began monitoring it in 2001.
Of concern is the fact that this study is based on pre-COVID-19 data.
“I think we have underestimated the impact of the pandemic on child and youth mental health,” says Dr. Peter Szatmari, chief, Child and Youth Mental Health Collaborative, CAMH. “It is an impact that is being referred to as a ‘shadow pandemic.’ The factors contributing to this negative impact include social isolation; the lack of opportunity to participate in the kinds of activities that bolster resilience and strength, such as sports, hobbies and other kinds of physical activities; and the opportunity to do well at school,” he says. “The impact of the pandemic on parents is also of significance. The losses accrue: the financial stress around a parent losing a job; the death of a family member due to contracting COVID-19. There are a number of accumulative pandemic factors that can be ascribed to this worsening of mental health and suicide ideation in youth.”
Death by suicide is the second most common cause of death in the youth cohort, an age group that ranges from six years to 24 years of age. In fact, suicidal behaviour, which includes suicide ideation, suicide attempt and completed suicide, represents, according to Dr. Szatmari, a higher number of suicide attempts in the youth cohort than in any other age group. The actual completion of death by suicide is higher in older people.
Increased isolation as a result of the pandemic lockdown, family issues around compromised finances, the backlash of stress from parents who are juggling both the new shelter-in-place working-at-home parameters, which require the ability to be technologically informed (something at which many parents might not be adept), as well as the challenges and unfamiliarity of helping their children with online learning, the loneliness from not being able to see and spend time with friends, the closing of schools and the resultant lack of day-to-day structure, inactivity, lack of access to outdoor activities, both in a school setting as well as with peer groups, have caused havoc with kids’ mental health. One of the ways these issues are manifesting is in the alarming rise of eating disorders in this age group.
“Suicidal ideation that lasts more than a day, more than a couple of hours, is a very serious thing that needs to be evaluated” — Dr. Peter Szatmari
“The pandemic overall is having a profound impact on mental health in children, youth and families,” says Kim Moran, CEO of Children’s Mental Health Ontario. “There have been huge increases in serious mental illnesses. For example, the Children’s Hospital of Eastern Ontario’s (CHEO) Eating Disorders Program has seen a 50 per cent increase in the number of emergency assessments since the beginning of the pandemic. In-patient admissions to CHEO between April 1 and Oct. 31, 2020, increased 63 per cent over the same period last year. Some of the virtual mental health clinics across the province have doubled their volumes in the past year, all signs that youth mental health is an issue,” she says. “When schools closed in March 2020, more than half of parents noticed behavioural changes in their child, including outbursts or extreme irritability, drastic changes in mood, persistent sadness or preoccupation, avoiding formerly enjoyable activities, including spending time with friends, and eating considerably more or less, all signs which suggest there are problems with the child’s mental health,” says Moran. “And certainly, we have seen research and evidence from around the world that shows similar issues of worsening mental health, suicidality, anxiety, depression and substance use in our youth, all related to the pandemic. We also know that marginalized, racialized and at-risk children who were already having trouble have been hit even harder.”
Addressing racialized communities which have historically been disenfranchised from social systems is something that David Willis, director of Toronto’s Lead Agency for Child and Youth Mental Health, System Transformation at Strides Toronto (which supports 26 mental health agencies across the GTA), identifies as being of critical importance to the mental well-being of the youth in that cohort.
“When the pandemic hit, there was an enormous drop in the utilization of our services,” Willis says. “But once the clinicians and programs became more adept at virtual delivery, we did see an incredible increase in the numbers of kids reaching out virtually.”
At the same time, however, Willis says that there has been a concerning drop in some of the Mental Health T.O. longer-term in-person programs, ones that involve the whole family, since the start of the pandemic.
“This decrease tells us that there are far more kids out there who are experiencing mental health issues, but are not reaching out. Because of the lockdown, these kids have become more isolated than they normally would be, and that is a huge worry,” he says.
And while the ideation of suicide is not uncommon in kids who are under stress, the actual attempt of doing so, or of harming oneself, needs to be taken seriously by both family members and friends.
“Suicidal ideation that lasts more than a day, more than a couple of hours, is a very serious thing that needs to be evaluated,” Dr. Szatmari says. “We tend to dismiss and underestimate the importance of these mental health indicators in children. We explain them away, we say things like, ‘Oh, it’s just a cry for help, or the person is trying to get attention,’ but that just isn’t true. These excuses are tied to the stigma of mental health, a stigma that is larger when talking about the mental health of our youth cohort than in other age groups.”
So where do we go to from here? What are the resources that can be accessed both by families as a whole and kids on their own?
“It is OK to reach out for help; it is not a weakness. In fact, it shows intense resilience, intense strength and emotional literacy” — Tamar Brannigan
While many of us are familiar with the “normal” or common access points to source mental health assistance, including emergency departments, counsellors, family doctors and community mental health centres, the opportunity for kids to access help on their own, to connect with qualified counsellors who understand and can help them — most especially for kids whose parents or culture do not condone “sharing secrets outside of the family unit” — is of critical importance, ones that young people need to be aware of.
Dr. Szatmari states that kids often don’t want to tell their parents they are suffering mentally and emotionally, because they don’t want to disappoint or worry them, especially at a time when their parents are also under undue stress.
“It becomes very difficult for some kids,” Willis says. “Their home environment might not be a safe place, so how do they reach out and ask for help?”
Tamar Brannigan, manager, Community Crisis Responders at Kids Help Phone, encourages kids to pick up the phone, reach out and not worry about any stigma they might feel is associated with asking for help.
“It is OK to reach out for help; it is not a weakness. In fact, it shows intense resilience, intense strength and emotional literacy,” Brannigan says.
The serious effects of the COVID-19 pandemic on the mental health of our youth are alarmingly evident in the increase of calls to Kids Help Phone during 2020.
“In 2020, we facilitated 4,200 active rescues with young people who were at risk of suicide,” Brannigan says. “If a young person is at imminent risk, we make sure they get the help they need.”
The stats are disturbing.
In 2019, Kids Help Phone had 1.9 million connections. In 2020, they had 4.5 million connections with young people through their phone line, text and website access points. This increase in connections, year over year, represents an alarming 137 per cent increase.
“It is important to note that while suicide is not always the intent of the crisis, when it does happen, 125 people are directly affected by that one suicide,” Brannigan says.
Interestingly, in addition to the free, 24-hour help line for kids, 1-800-668- 6868, Kids Help Phone has opened up a free accessible service for adults as well: 741-741.
“These are really tough times, and parents are under a huge amount of stress. They are frustrated and wearing so many hats, they are virtually at the end of their rope,” Brannigan says. “Our 741-741 service is for both parents and adults in general, a means and a resource to reach out and to access crisis support and help. They will be connected with a counsellor who will provide non-judgmental support.”
Dr. Szatmari agrees that the mental health of parents is having a huge impact on the mental health of their children.
“If parents are more stressed and experience more anxiety and more depression and more substance use as a result, that is going to affect their kids, because they are not as available for their kids to support them and help them deal with their stresses,” he says. “It is a vicious cycle: the more that kids get depressed and anxious, the more parents are impacted. Unless there is something that breaks the cycle, the situation can rapidly deteriorate.”
The What’s Up Walk-In Clinics, with six locations in the GTA (and branded throughout the rest of the province as Brief Walk-In Services), is a resource that youth can virtually walk into to access help (pre-COVID-19). Usually scheduled over one or two sessions, it is a service which helps kids and counsellors identify and mitigate problems, so that they don’t become bigger issues going forward.
“When a kid accesses our free Brief Walk-In Services (which are under the Mental Health T.O. umbrella), they don’t even need a health card,” Willis says. “They can literally show up, give a bit of brief information about themselves and what is going on, and within 20 minutes they are hooked up with a clinician for a 90-minute session.”
As schools and small businesses inch toward reopening, albeit under highly strict protocols, the question that resonates across all age cohorts is: “Where do we go from here?”
The fact that kids are going back to school is one that, although it might present some worry and angst around the transmission and contraction of the virus, is also one that is viewed by parents, many medical experts and the kids themselves as being a concrete step toward a more positive sense of well-being.
“School plays a very important role in early identification of children who have a mental health issue,” Moran says. “Teachers and administrators are well trained to see if a child is struggling and then navigate them to care. Of course, these networks have decreased substantially, because school isn’t in place.”
The importance of opening schools so that kids can feel less isolated and get back to a normal routine is one that Dr. Szatmari strongly supports.
“The evidence of transmission of the virus in children is pretty low,” he says. “If we can make schools a safe environment from a health point of view, we should encourage and support opening them.”
In addition to the opening of schools as a way to reboot the normalization of life for kids, the questions and complex issues that need to be considered and addressed once this pandemic is over are many: “What is the new normal going to look like once we have all had the chance to be immunized? What are the ongoing hidden emotional effects on all of us — youth, parents, adults in general? What are the lasting effects? How is society going to change?”
“What is the new normal going to look like?” Dr. Szatmari asks. “I think we need to be prepared to be vigilant; we can’t let our guard down, like we did prior to the onset of COVID-19. None of us was prepared for the mental health impact of this pandemic when it started a year ago, and that was a mistake. I think we’ve learned from that, but we need to be vigilant. We need to increase the resources that are devoted to mental health in general and to child abuse mental health, in particular,” he says. “We spend much less money on mental health than we do on physical health, but, in reality, disability and quality of life are affected by mental health to a much greater extent than they are by physical health. In general, we need to put more resources into mental health, in particular, kids’ mental health, in order to support them.”
As a society, each and every one of us has been distracted by the unfamiliar — what is famously called “unparalleled and unprecedented” effects of the COVID-19 pandemic. Nonetheless, we each need to be aware and pay attention, in a mindful and present manner, to what our children and young adults are feeling.
Family bonding can take on many forms: we can cook or bake together; go on family walks or toboggan down the nearest hill; we can imagine a family vacation once the pandemic is over; or we can play games that include everyone.
“The most important thing is to fight against the social isolation,” Dr. Szatmari says. “Find innovative ways of being together in a healthy way, whether that’s on the internet or over the phone or going for walks at a distance from each other. We need to be present — truly present — to be together in some way. I think that promoting social relationships in a healthy way is the most important ingredient to being resilient against the stresses of this pandemic.”
As Ontarians move backwards through the COVID-19 colour-coded response framework in place throughout the province, that is, from grey (lockdown), to red (control), to orange (restrict), to yellow (protect) to green (prevent), it is important for the youth cohort to know that the resources for their mental health are available, on a non-judgmental basis, and are free and accessible 24-7, without the need or complication of a health card.
“I want to encourage both kids and parents to reach out and talk to someone outside of the home, whether that is a friend, a counsellor or a crisis service. There are resources out there,” Brannigan says.
Access Kids Help Phone for free at 1-800-668-6868 for counselling sessions in English, French and Arabic.
“We need do a better job the next time the next pandemic comes along, because you can be darn sure there’s going to be another one,” Dr. Szatmari says.