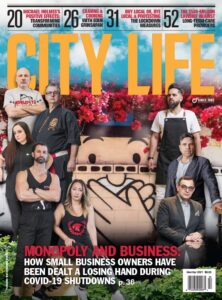
How 4 Covid-19 Survivors Touched Death
COVID-19 is a virus infecting and killing people all over the world. Based on scientific research, the novel coronavirus appears to produce different symptoms, depending on an individual’s pre-existing conditions and genetics. Pages from the ‘COVID-19 Diaries’ talk one-on-one with survivors of the deadly virus, revealing their incredible triumphant stories.
More than eight million people worldwide have become infected with COVID-19 and more than 435,000 have died. Whether you’re a front-line worker or you’re living in a seniors’ residence, this virus doesn’t play favourites. Over the last three months, it has infected more than 32,000 people in Ontario and killed more than 2,500.*
The following are stories from people who stared down COVID-19, took its punishment and lived to tell their tale.
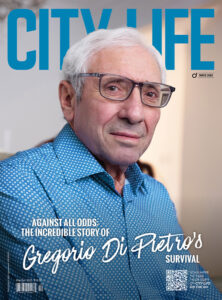
THE POWER OF PRAYER
Mario Bottoni is a 55-year-old businessman from Kleinburg, Ont. Originally from Italy, he immigrated to Ontario as a teenager. He was raised as a Roman Catholic, always cherishing his special relationship with Jesus. A week before he was jettisoned to North York General Hospital’s (NYGH) emergency ward for a suspected heart attack, he had a vision. “I experienced a premonition that I would be hospitalized and shared this with my family. I advised friends, family members and neighbours to place a crucifix at their main door entrance to signify their faith.”
On March 24, Bottoni had been in a business meeting with his lawyers and accidentally shook one of the associate’s hands. The following day, he discovered the associate had tested positive for COVID-19. Shortly after, Bottoni became feverish, had a mild cough, a sore throat and felt like he was having a heart attack. “On April 1, I was driven by my wife to NYGH. Once in the hospital, I was immediately induced into a coma and put on a ventilator.” Bottoni still has flashbacks. “While in the coma, I felt a heavy weight removed from my soul and was comforted by a power I’d never felt before, as my right hand was held by Jesus or sacred Mother Mary. What is certain is that I was never alone and no longer scared.” When he finally awakened after almost four weeks in a coma, he was diagnosed with intensive care unit (ICU) delirium. He had no idea where he was or what year it was. Dr. Pascal, the head physician who took care of Bottoni, later informed him that “the odds of survival after four weeks on a ventilator are very slim.” Studies suggest more than two-thirds of people die while on ventilators. While Bottoni was now breathing on his own, the fight for his life was just beginning. His kidneys had also been badly damaged during the virus, and he was hooked up to a dialysis machine. “On May 1, I prayed with the rosary on my knees for two hours, as I was not urinating and went from 20 millilitres to 1.5 litres throughout the night. I was overwhelmed with joy and believed my prayers were answered.” By May 5, Bottoni was finally discharged. As he left the hospital, hundreds of staff stopped, turned and gave him a standing ovation. During his stay at the NYGH, he indicated that friends and family from all over the world were praying for him. One friend in particular who prayed for his soul was a man who’d been like a spiritual guide to him for years, Father Buona Michel Rouhana, from Beirut, Lebanon. As soon as Father Rouhana found out Bottoni was ill, he called and emailed the family constantly. He gave them hope and a reason to believe Bottoni would beat COVID-19. “I believe all the prayers from family, friends and prayer groups from all over the world brought me home to my family, and [it is] only because of the support by so many people and my deep relationship with God our saviour, Jesus and Mother Mary that I survived the horrible disease.”
While in the coma, I felt a heavy weight removed from my soul and was comforted by a power I’d never felt before, as my right hand was held by Jesus or sacred Mother Mary. What is certain is that I was never alone and no longer scared — Mario Bottoni
ADVOCATE
Dale Feinstein, a single mother in her mid-40s, has no idea how she contracted the killer virus. “On April 4, I suddenly lost all sense of taste and smell.” At this point, Feinstein contacted an ear, nose and throat (ENT) specialist, who told her that she should get tested and self-isolate immediately. Subsequently, Feinstein called Telehealth, which acknowledged most likely that doctors wouldn’t test her, since her symptoms at the time weren’t listed. Feinstein called the ENT doctor back, and he immediately referred her to the testing clinic in his hospital. She felt like she was in the Twilight Zone. The doctor at the clinic also didn’t think she needed a test, but Feinstein, who’s no shrinking violet, demanded one. Two days, later she received a call from the clinic. She had tested positive for COVID-19. Today, Feinstein has recovered, but if it weren’t for her non-stop persistence, she wouldn’t have been tested. She’s afraid others won’t advocate for themselves. “I know how to push, and I am very assertive. Many people are quick to take “No” for an answer and are uncomfortable about advocating for themselves.”
Dr. Andrew Morris, an infectious disease specialist at the University Health Network and Mount Sinai Hospital in Toronto, explains why everyone in Ontario can’t be tested: “Ideally, we would be testing many more people than we are. In Ontario, we have a limit on the number of tests we are able to perform each day. At the time of writing, that appears to be 18,000 tests,” he says. “We have about 15 million people in Ontario. Just because someone wants to be tested, doesn’t make it the best use of testing resources at present. I remain concerned about our capacity for testing. It is inadequate, but in the meantime, we need to be strategic about who we test.”
COVID-19 FEAR
Zale Newman and his wife Rachel’s journey into hell started on March 21, when they both tested positive for COVID-19. Zale remembers: “A week later, Rachel was unable to retain liquid and was very nauseous, so I took her to NYGH for intravenous and nausea treatment.” At NYGH, she was immediately taken to the ICU ward. By 1 a.m., Zale received a call he’ll never forget. “My wife had consented to being put into an induced coma, so staff could insert a breathing tube down her throat and attach her to a ventilator.” For 11 days, Rachel was in a coma and hooked up to a breathing machine, while Zale was unable to visit and had no idea whether his wife would survive. “When she awoke from the coma, she had post- ICU delirium. She didn’t know where she was, what year it was, the month or the day,” says Zale. Once Rachel awoke from the coma, she was quickly relocated to another unit in the hospital. Says Zale: “She was in isolation and not allowed to leave from Wednesday to Saturday.” Reflecting on her situation, Rachel says that “sometimes I would just walk out of my room and say, ‘Is there a nurse here?’ Then I’d hear someone yell, ‘Get back into your room now. You’re not to leave your room.’
No one had explained to me I might be contagious.” Two and a half weeks later, Rachel was discharged. When Zale arrived at the hospital to pick her up, “her clothes were in a bag, and they were in a hurry to get her out of the hospital. COVID[-19] fear reigned. My wife was delivered to the exit in just a hospital gown.” As Rachel left, hospital staff provided Zale with a list of the medications she was taking. “No one from the ward, no doctor or nurse, no exit interview, no one ever spoke to me,” he says. Back at home, Zale attempted connecting with several doctors who refused to see his wife, because “the government didn’t provide them with enough PPE equipment.” Finally, with his wife writhing in pain on the floor due to digestion and dehydration issues, he connected with his sister, a former nursing professor in Israel. She sent them a series of instructions to improve Rachel’s physical health. As Rachel started to see a glimmer of hope, Zale realized she was also experiencing severe mental illness. “We used connections to arrange for her to see a top post-traumatic stress disorder [PTSD] doctor at Mount Sinai and a doctor from Sunnybrook — all things that NYGH could have provided.” Nadia Daniell-Colarossi, a North York General Hospital spokesperson, says she cannot comment on individual patients, but “it is distressing to hear when patients and families experience any kind of gap in care. And it is important for us to know when we have not met their needs. We, of course, want to have open and direct conversation with our patients and their families, so we can understand and address their concerns.”
We used connections to arrange for her to see a top post-traumatic stress disorder [PTSD] doctor at Mount Sinai and a doctor from Sunnybrook — all things that NYGH should have provided — Zale Newman
Even though the Newmans were disappointed with the help they received after leaving the hospital, both Zale and Rachel were quite impressed with the care Rachel received while in the ICU. “We gave them snack cards from Tim Hortons at the hospital twice for all of the ICU staff, and about two weeks ago, we arranged for meals to be sent in for all of the ICU staff members,” says Zale.
Toronto psychotherapist Karen Dougherty says the psychological ramifications for patients who have survived COVID-19 are severe. “Being in ICU on a ventilator is extremely traumatizing at the best of times. But being on a ventilator with COVID-19 is far worse. In part, that’s because of the isolation, the terror, fear of death, sedation and so on. There is very little to orient the patient in reality, time and space, because they can’t have visitors, and doctors and nurses are in full personal protective equipment.” Says Dougherty: “There can be ICU delirium, which can involve paranoia and vivid hallucinations. Our ability to tell real from imagined is compromised. This can leave us traumatized. Therapy can really help people who have suffered through this, to stave off PTSD, which may include the following symptoms: nightmares, panic attacks, flashbacks, terrible anxiety and depression.”
WINNING THE WAR
Whether this pandemic continues for another six months or two years, Canadians have shown they have tremendous resilience. Whether we’re on a ventilator, whether no one will test us or our symptoms keep worsening after we’ve been declared stable, Canadians are proud warriors who won’t give up. We’ll drop our sticks and gloves and keep on fighting until the final buzzer.
*These numbers are accurate at the time of print.